Psoriatic Arthritis
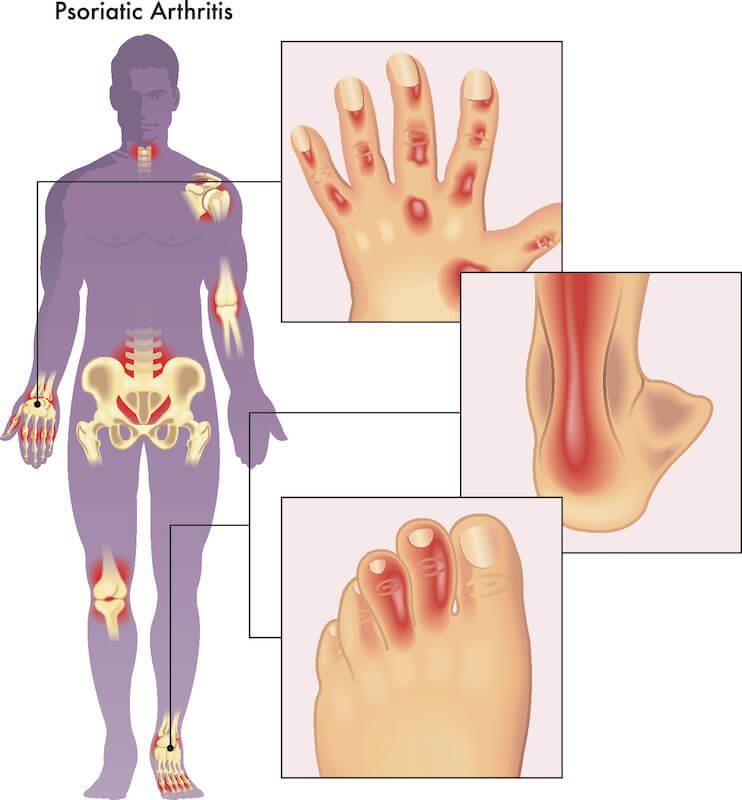
Psoriatic arthritis is an inflammatory form of arthritis affecting psoriasis patients. Chronic arthritis can cause joint pain, rigidity, edema, and fatigue. Joint pain and edema are early indicators of psoriatic arthritis, particularly in the digits and toes.
Before experiencing joint symptoms, individuals with psoriasis may observe their nails becoming pitted or detaching from the nail bed. Other early symptoms may include difficulty moving joints and stiffness after prolonged reclining. Some patients with psoriatic arthritis may also experience tenderness or discomfort where tendons and ligaments adhere to the bones.
Those who suspect they may have psoriatic arthritis should immediately seek medical attention. Early diagnosis and treatment can help manage symptoms and halt the progression of joint injury. Medication to reduce inflammation, physical therapy to enhance mobility and strength, or adjustments in lifestyle, such as weight loss or stress management techniques, may be used to treat inflammatory bowel disease.
Symptoms: Skin, Joints, Nails
Skin, joints, and fingernails are three areas of the body that can indicate the onset of psoriatic arthritis. A silvery-white rash or patch on the epidermis is one of the most prevalent symptoms. The most common locations for these patches are the elbows, knees, cranium, and lower back, but they can appear anywhere on the body. In addition to these regions, some individuals also experience itchy or scorching skin.
Additionally, psoriatic arthritis is also characterized by joint inflammation and edema. This form of arthritis causes inflammation in the joints, which can cause stiffness and discomfort that is worse in the morning or after prolonged sitting. The affected joints may also feel heated to the touch and turn red.
Changes in the cuticles may also serve as an early indicator of psoriatic arthritis. Nails may begin to separate from their beds or develop ridges or depressions on their surface. They could also alter their form or become discolored, with yellowish-brown patches appearing beneath them. It is essential not to disregard these changes, as they may indicate underlying joint problems caused by psoriasis-associated inflammation.
Diagnosis: Blood Tests, Physical Exam
With the aid of blood tests and physical examinations, the first indicators of psoriatic arthritis can be detected. Psoriasis increases the likelihood of developing psoriatic arthritis, a chronic autoimmune disease that causes joint pain, rigidity, and inflammation. It can result in permanent joint injury if left undiagnosed or untreated.
Inflammation and other possible indicators of psoriatic arthritis can be detected through blood tests. In addition, they can rule out other conditions that may present with similar symptoms. Joint sensitivity, edema, and range of motion are evaluated during physical examinations. This enables physicians to detect any abnormalities or deformities in the joints, which may indicate psoriatic arthritis.
Treatment options are more effective in the early phases of psoriatic arthritis, making early diagnosis crucial for disease management. If you have joint pain or swelling, particularly if you have previously been diagnosed with psoriasis, you should visit your doctor immediately so he or she can order blood tests and perform a physical examination to check for signs of psoriatic arthritis.
Treatment: Medication Management
Medication management is an essential aspect of care for the treatment of psoriatic arthritis. Early symptoms include joint pain, rigidity, and edema, which can be treated with nonsteroidal anti-inflammatory medications (NSAIDs). These medications alleviate pain and inflammation, making it simpler for patients to move about and perform daily tasks.
In cases of psoriatic arthritis that are more severe, disease-modifying antirheumatic medications (DMARDs) may be prescribed. These medications suppress the immune system and reduce joint damage to be effective. Patients who have not responded favorably to other treatments may also be administered biologic therapies. Specific proteins that contribute to inflammation within the body are targeted by biologics.
It is essential for patients to collaborate closely with their healthcare provider when managing their psoriatic arthritis medication regimen. On the basis of a patient’s response and adverse effects, it may be necessary to conduct periodic checks and make adjustments. By taking their medications correctly, people with psoriatic arthritis can enhance their quality of life and manage their symptoms.
Complications: Increased Risk of Infection
Early symptoms of psoriatic arthritis are frequently misdiagnosed as rheumatoid arthritis or gout. However, an increased risk of infection is one of the main complications that distinguish psoriatic arthritis from these other conditions. This is because psoriasis patients have abnormally functioning immune cells that can attack healthy tissue, leaving the body vulnerable to infection.
People with psoriatic arthritis are more likely to contract an infection, and if they do, they may experience more severe symptoms. Due to the compromised state of their immune system, they may have a difficult time fending off the infection. Persons with psoriatic arthritis must take extra precautions to avoid infections, such as routinely cleansing their hands and avoiding contact with ill individuals.
Although an increased risk of infection may be a complication of psoriatic arthritis, it is crucial to consider that you can take steps to reduce this risk and maintain your health. By remaining aware of your body and taking the necessary precautions, you can keep yourself secure and effectively manage your condition.
Coping Strategies: Physiotherapy, Stress Reduction
Physiotherapy can help individuals with early psoriatic arthritis symptoms manage their symptoms. This type of rehabilitation is intended to help individuals regain normal physical function and maintain it, as well as prevent further injury.
Physiotherapy for psoriatic arthritis may include exercises that increase joint mobility and strengthen muscles near the affected area. Physiotherapists can also instruct patients on proper posture, body mechanics, and ergonomics, which can reduce joint stress.
Reducing stress is another essential coping strategy for those with early psoriatic arthritis symptoms. It has been demonstrated that stress aggravates the symptoms of this condition, such as pain and inflammation.
Meditation and thorough breathing can help patients effectively manage their tension levels. In addition, regular physical activity, such as yoga or Pilates, can help reduce tension and enhance your overall health and well-being.
Conclusion: Early Detection Benefits
Early detection of psoriatic arthritis can greatly benefit patients in terms of disease management and pain reduction. By recognizing the earliest signs and symptoms of this condition, patients can treat it with the appropriate medication, physical therapy, and lifestyle modifications. Additionally, early detection may prevent joint injury that could result in permanent disability.
If patients with psoriatic arthritis are diagnosed and treated early, before their symptoms worsen, they may also have an improved prognosis. This can also save money on health care, as costly surgeries and treatments will not be required as frequently as when the disease is left untreated for an extended period of time.
Conclusion: Recognizing the early symptoms of psoriatic arthritis is essential for preserving a patient’s quality of life and preventing long-term complications. Therefore, individuals with any probable symptoms should consult their physician immediately so that they can begin treating this condition as soon as feasible.

